
CHILDREN’S HEALTH INSURANCE PROGRAM CHIP
Is CHIPS Medicaid
The children’s Health Insurance Program (CHIP) come about from the provisions of the Balanced Budget Act of 1997 (BBA).
It seeks to address health insurance coverage gaps that are faced by children in needy households covered by Medicaid (who earn too much to qualify for Medicaid but not enough to buy private insurance) and the well-off households that can afford private health care plans.
The CHIP program is structured as a federal-state partnership. However, States are at liberty to set up their own CHIP programs (can set their own eligibility levels and cost-sharing requirements in their programs).
This state arrangement can either be as an extension of Medicaid, CHIP-Medicaid partnership, independent program, or as a separately branded program. In some states, CHIP provides coverage for pregnant women.
CHIP Coverage
Its benefits vary across states. But all the states do provide comprehensive coverage (must include Early, Periodic Screening, Diagnosis, and Treatment (EPSDT) or any similar standard of care as prescribed by the federal government). This includes:
- Preventive Routine care and check-ups
- Immunizations and vaccinations
- Doctor visits
- Medical Prescriptions
- Dental care and vision evaluation(including eyeglasses)
- Inpatient and outpatient hospital care
- Lab and X-ray
- ER services
Coverage for CHIP can begin immediately, and at any time of year.
Is CHIP costly
There is no charge for Routine “well child” doctor and dental visits under CHIP. Though, you may be charged copayments for other services.
Some states have a monthly premium charge for CHIP coverage. These costs vary across states, but can’t be more than 5% of a household’s income for that year.
Infants born to women who are eligible for Medicaid, some children in foster homes or adoption programs, and some disabled children may also be eligible for CHIP regardless of income.
Financing for CHIPS Program
Congress authorizes and appropriates annual allotment of funds which is distributed to the individual states to finance their CHIP program. CHIP funding is capped and also is considered mandatory spending. Congress provides funding for multiple years at a time.
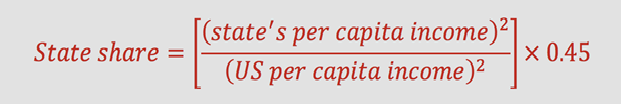
States’ share of total federal appropriation for a specific year is based on;
- State’s historical program expenditures,
- growth in a state’s child population,
- Total growth in national health care expenditure, and
- The Federal Medical Assistance Percentage (FMAP)
The FMAP determines the federal funding match rate for the state Medicaid program. This encourages states to create or expand children’s coverage.
States typically may roll over any unspent funds from one year to the next, though Congress sometimes rescinds at least a portion of unspent funds.
CHIP eligibility
Young people up to 21 may also be eligible for Medicaid. Youth includes children who have “aged out” of their parents’ plan and can be covered under Medicaid (not covered through a group health plan or creditable health insurance). This safety net lasts until they reach 26 years; the CHIPS program does not have an income limit for “aged out” children.
Eligibility depends on several factors, this includes:
-
Income level and Age
Modified adjusted gross income (MAGI), which is a tax-based measure of income is used to determine an applicant’s eligibility for Medicaid and CHIP. Taxable income and tax filing relationships are considered to determine eligibility.
The different States have their own income eligibility rules, but most states, qualify children up to age 19 with family income up to $50,000 per year (for a family of four).
In some states, the family income may be even higher but still, children still qualify (the fact that both parents are working doesn’t necessarily mean coverage is accessible through their employer-based plans).
-
The size of the household
Generally, household size is determined by the tax filers and their tax dependents in a household. Different family members may be included in an individual’s Medicaid and CHIP household size especially when determining eligibility for someone who doesn’t file a tax return and is not claimed as a tax dependent.
-
The Individuals age, pregnancy status, and whether they have a disability
The target is to provide coverage to certain groups that have been historically excluded from CHIP, such as low-income children or low-income pregnant women that are lawfully residing, or have access to public employee coverage
-
State requirements
The family or household must be residents of the state
-
Immigration status
Medicaid and CHIP coverage is for U.S. citizens and certain lawfully present immigrants.
It should be noted that having Medicaid or CHIP cannot affect someone’s path to becoming a Lawful Permanent Resident or U.S. citizen.
CHIP Vs Medicaid
Although the ACA sets the minimum requirements (as it seeks to create a continuum of coverage)across all healthcare plans, some differences still exist in the way Medicaid for children and CHIP are handled at the state level.
Matching Funds
The federal government matches state spending for Medicaid and CHIP. However, the CHIP match rate (71%) is higher than the Medicaid match rate (56%).
Medicaid has no pre-set limits or caps for federal matching funds but Under CHIP, matching funds are capped and the states are limited to their specific allotment of funds.
Coverage Requirements (as per the Federal regulations mandate)
Far fewer restrictions exist in the formulation and operation of separate CHIP programs. Dental care offered may not be as extensive as that offered under Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) and must be part of the included benefit package. On the other hand, Medicaid has higher minimum comprehensive coverage requirements and includes EPSDT services.
Also, Services covered by Medicaid services include care provided at Federally Qualified Health Centers (FQHCs) and rehabilitation services.
States have the liberty to design CHIP coverage around its minimum coverage requirements and may choose to include benefits covered under Medicaid.
Cost Sharing
Under Medicaid, states cannot charge premiums and cost-sharing for mandatory coverage. On the other hand, States with a separate CHIP program are allowed to impose premiums and cost-sharing.
CHIPS Medicaid Income Limits
Eligibility levels range between 138% and 405% of the federal poverty level (FPL) and vary from state to state.
30 states’ have capped their eligibility levels to between 200 percent and 300% FPL, while 19 states have set their eligibility levels above 300% FPL.
States with a cap higher than 300% FPL may lose their E-FMAP and will only receive the regular Medicaid FMAP for CHIP enrollees above 300% FPL.
More than 97% of CHIP enrollees have a family income of below 250% FPL.
Comprehensive CHIP and Medicaid eligibility levels are found on the Medicaid and CHIP Eligibility Levels page.
Medicaid CHIP Application
Each state program has its own eligibility rules, and applications can be made via state agency at any time of year.
You have 2 options when applying for CHIP:
- By Calling 1-800-318-2596 (TTY: 1-855-889-4325) or by Visiting your state’s website.
- Fill out and submit an application through the Health Insurance Marketplace. If anyone in the household is eligible for Medicaid or CHIP, this information will be relayed to the state agency who will in turn contact the applicant regarding enrollment.
By submitting a Marketplace application, you get to know if your children are eligible for CHIP (if they do, you won’t have to buy an insurance plan to cover them).
You will also get to find out if eligible for an individual insurance plan with savings based on your income instead.
Coverage may begin immediately or may be effected retroactively.
Medicaid CHIP Enrollment
Special Enrollment Periods (SEP) for Medicaid and CHIP are open to individuals who;
- Have lost their Medicaid or CHIP coverage (including pregnancy-related coverage and medically needy coverage or aging out of CHIP coverage). Access to SEP is by making an application at the Marketplace and attesting to this loss of coverage.
- Had applied for coverage at the Marketplace or through their state agency during the Open Enrollment Period (OEP) and were determined ineligible after the close of OEP ended. Access to SEP may be via submitting a HealthCare.gov application and attesting to their denial.
- Made an application for coverage through the Marketplace following a SEP Qualifying Event, and were assessed as potentially eligible for Medicaid/CHIP, but were determined ineligible more than 60 days after the original SEP qualifying event.
- Have become just eligible for help paying for Marketplace coverage when moving to a new state, and/or experienced a change in income or Ineligible because they lived in a state that hadn’t expanded Medicaid.
- Are Ineligible for help because their household income was below 100 percent of the FPL. They can access this SEP by calling the Marketplace Call Center and explaining your current situation.
If an individual qualifies for SEP, they generally have 60 days after the qualifying event to make changes- make a new selection or change current Marketplace coverage.
Enrollment Strategies
Express lane eligibility (ELE)
It’s a simplified process for determining/re-determining CHIP and Medicaid coverage eligibility.
States that use ELE can rely on appraisals for eligibility done by another program designated as an express lane agency to facilitate enrollment.
Express lane agencies may include:
- Supplemental Nutrition Assistance Program,
- Temporary Assistance for Needy Families,
- Head Start,
- National School Lunch Program, and
- Women, Infants, and Children.
Continuous Eligibility
States have the choice of providing children with 12 months of continuous coverage under CHIP and Medicaid. This is done even if the family has experienced changes in income during the year.
Presumptive Eligibility
States also have a choice of implementing presumptive eligibility.
States do use title XXI funds to cater for costs of CHIP coverage during the period of presumptive eligibility. This is pending the actual screening process that will lead to final eligibility determination.
Bottom Line
Medicaid and CHIP programs are open for enrollment all year-round.
Renew annually to maintain continuous coverage. Also, Ensure contact information is up to date so as not to miss important notices which can easily lead to gaps in coverage.
Children and teens can access CHIP coverage regardless of family income. CHIP does not have an upper-income limit. They can be enrolled in free, low-cost, or full-cost CHIP.
Children with this coverage have better access to medical care than uninsured children. This care can be easily compared to private insurance plans.
Most households qualify for CHIP at no cost. Some households with incomes falling below the CHIP threshold may qualify for Medical Assistance. However, Households with higher incomes may have access but with low monthly premiums and copays.
Leave a Reply
You must be logged in to post a comment.